High blood pressure, or hypertension, is one of the most common health conditions worldwide. It means the force of blood against your artery walls is consistently too high, making your heart work harder. Over time, this can quietly damage your body. Hypertension is a significant health concern affecting nearly half of American adults. Yet many people with high blood pressure don’t even know they have it, earning hypertension the nickname “the silent killer.” Early detection and management are crucial because uncontrolled high blood pressure can lead to serious problems. In this article, we’ll explain what hypertension is, why it matters for your health, and how a functional medicine approach can help you manage or even reverse it through root-cause solutions and lifestyle changes.
What Is Hypertension and Why Is It Important?
Hypertension simply means chronically high blood pressure. Blood pressure is measured with two numbers (like 120/80 mmHg, spoken “120 over 80”). The top number (systolic) is the pressure when your heart beats, and the bottom number (diastolic) is the pressure when the heart relaxes between beats. For healthy adults, normal blood pressure is around 120/80 or below. Doctors typically diagnose hypertension when readings stay above about 130/80 to 140/90 mmHg over time.
Hypertension matters because it puts extra strain on your heart and arteries. If left unchecked, high blood pressure significantly raises the risk of serious health issues. It is a leading cause of heart attacks and strokes, and contributes to heart failure, kidney damage, vision loss, and other problems. The constant pressure can damage blood vessels throughout your body, affecting organs like the heart, brain, kidneys, and eyes. In fact, chronic hypertension is strongly linked to cardiovascular diseases such as coronary artery disease and can even lead to dementia or memory loss over time. By controlling blood pressure, you dramatically lower your risk of these life-threatening complications.
Symptoms: The “Silent” Condition
One of the tricky parts of hypertension is that it often has no noticeable symptoms. Most people feel perfectly fine even when their blood pressure is high. That’s why hypertension is frequently called a “silent condition” – you usually don’t know it’s there until it’s found during a check-up. Many discover they have high blood pressure only when a doctor measures it or when a complication (like a stroke or heart attack) occurs. Occasionally, if blood pressure climbs extremely high (e.g. 180/120 mmHg or above), a person might experience warning signs such as headaches, dizziness, blurred vision, chest pain, or shortness of breath.
Regular blood pressure screenings are very important, especially if you have risk factors. Checking your blood pressure is simple and it’s the only reliable way to know if you have hypertension. Staying informed about your blood pressure helps you catch hypertension early and take action before serious damage is done.
Causes and Risk Factors of High Blood Pressure
In the majority of cases, high blood pressure develops gradually due to a combination of lifestyle factors and genetics. This common form is called primary (essential) hypertension, and it isn’t tied to one specific underlying disease. Key risk factors that make you more likely to develop hypertension include an unhealthy diet (especially one high in salt and processed foods), lack of exercise, being overweight, smoking, heavy alcohol use, chronic stress, and older age. Family history and genetics do play a role, but interestingly, experts suggest that genes account for only a small percentage of hypertension cases. This means most high blood pressure is related to lifestyle and environment and therefore can often be improved by healthy changes.
In a minority of patients, high blood pressure is caused by an identifiable medical issue – this is called secondary hypertension. Some examples include kidney diseases, hormonal imbalances (such as an overactive thyroid or adrenal gland disorders), obstructive sleep apnea, or certain medications. These conditions can drive blood pressure up. If such a root cause is treated (for instance, correcting a thyroid problem or addressing sleep apnea), the blood pressure often improves. For most people, though, there isn’t a single “disease” causing hypertension – it’s the cumulative effect of diet, lifestyle, and overall health.
Functional Medicine: Addressing the Root Causes
Traditional medical treatment for hypertension often relies on medications to lower blood pressure. While medications can be life-saving and important, they don’t really fix why your blood pressure is high – they mostly manage the symptoms (the numbers). Functional medicine offers a different, more holistic approach. It asks: “What are the underlying causes of this person’s high blood pressure?” and “How can we address those causes to restore balance?” Instead of viewing hypertension as an isolated problem, functional medicine looks at your body as an interconnected system. By identifying the root causes – which can vary from person to person – and addressing them, the goal is to improve blood pressure naturally and sustainably, often reducing or even eliminating the need for medication.
In functional medicine, hypertension is seen not just as “high numbers” but as a clue that something in the body is out of balance. Practitioners will take a detailed look at your diet, lifestyle, stress levels, metabolic health, and even things like your gut and hormone levels. They may do specialized tests to uncover hidden contributors to high blood pressure (for example,
checking for inflammation markers, signs of insulin resistance, cortisol levels for stress, or imbalances in your gut microbiome). By treating these underlying issues, blood pressure often improves as a side effect of getting healthier! Below are some of the common root factors that a functional medicine approach might explore:
- Chronic Inflammation: Inflammation isn’t just about sore joints or infections – even low-level systemic inflammation can affect blood pressure. When your body is in an inflammatory state, the lining of your blood vessels (the endothelium) gets irritated and doesn’t function optimally. This can cause arteries to stiffen and narrow, raising blood pressure. Functional medicine practitioners look for sources of inflammation (such as a poor diet, chronic infections, or gut imbalances) and work to calm that inflammation with dietary changes and nutrients.
- Chronic Stress: It’s no surprise that stress can drive up blood pressure – we’ve all felt our heart pound during a stressful moment. When stress becomes chronic, your body stays in “fight or flight” mode. This means stress hormones like cortisol and adrenaline remain elevated, which makes your heartbeat faster and blood vessels constrict (tighten). Over time, this constant state of high alert contributes to persistently high blood pressure. A functional medicine approach puts a big emphasis on stress management.
- Insulin Resistance: A common (and often silent) contributor to hypertension is insulin resistance – a condition where the body’s cells don’t respond well to insulin, leading to higher blood sugar levels. Insulin resistance is usually tied to diets high in refined carbs and sugar, inactivity, and excess body weight (especially around the waist). You might know it as part of “metabolic syndrome” or pre-diabetes. This condition doesn’t just affect blood sugar; it also impacts blood pressure. Insulin resistance can drive up blood pressure by causing the kidneys to retain more salt and water and by increasing arterial stiffness. Many people with hypertension have underlying insulin resistance even if they haven’t been diagnosed with diabetes. The functional medicine solution is to improve insulin sensitivity through diet and exercise. As insulin resistance improves, often blood pressure comes down alongside it.
- Gut Health: It might surprise you, but your gut health – the balance of bacteria and overall function of your digestive system – can influence your blood pressure. How? The trillions of microbes in your gut play a role in regulating inflammation, producing certain nutrients, and even generating chemicals that affect blood vessels. Imbalances in the gut microbiome (dysbiosis) have been linked to higher inflammation in the body and even directly to hypertension. An unhealthy gut might contribute to the development of high blood pressure by triggering chronic inflammation or reducing the production of important molecules. By fixing gut issues, we reduce one more source of blood pressure trouble.
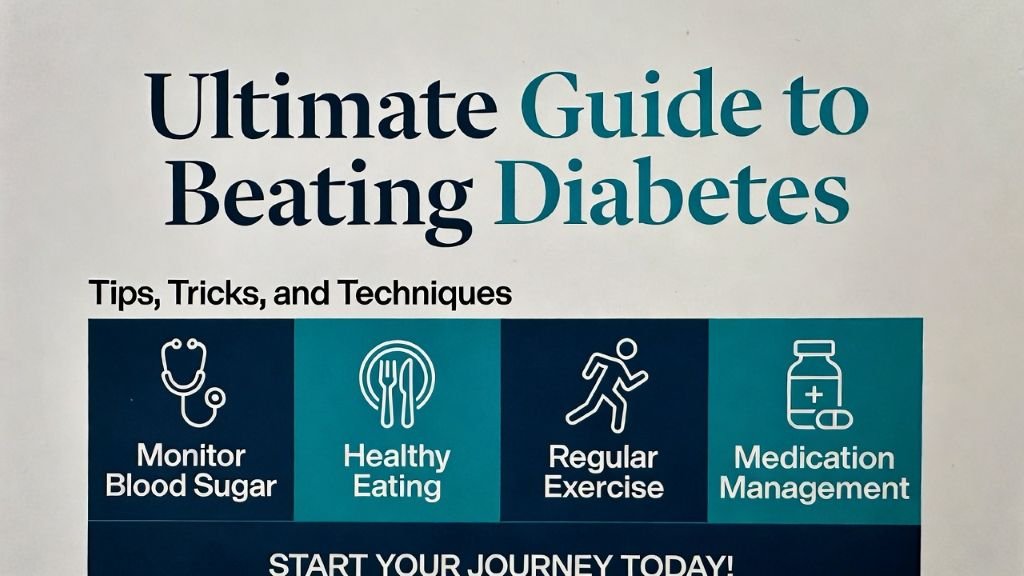
Key Lifestyle Interventions for Managing Hypertension
Lifestyle changes are the first line of defense in a functional medicine approach to hypertension. The empowering thing is that you have control over many of these factors. By adopting healthier daily habits, you can significantly lower your blood pressure naturally. In fact, clinical guidelines agree that lifestyle modifications are essential for anyone with high blood
pressure, and they can be powerful enough to bring mild hypertension down to goal levels without medication. Here are some of the key lifestyle interventions to focus on:
Nutrition: Eat Your Way to Lower Blood Pressure
Diet is perhaps the most powerful tool you have for managing blood pressure. A heart-healthy, nutrient-dense diet can directly improve hypertension. One proven approach is the DASH diet (Dietary Approaches to Stop Hypertension) – which emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats – or the similar Mediterranean diet. These diets are naturally high in potassium, magnesium, fiber, and antioxidants, and low in sodium and processed foods. They have been shown to reduce blood pressure in people with hypertension. In a functional medicine context, an anti-inflammatory diet is recommended. That means focusing on whole, unprocessed foods – lots of colorful veggies and fruits, nuts and seeds, fish and plant-based oils, and minimal sugar or refined grains.
Overall, eat plenty of whole plant foods and lean proteins, and minimize processed foods high in salt, sugar, and unhealthy fats. This not only helps blood pressure but also supports weight management and overall cardiovascular health. And don’t forget to drink water and stay hydrated – dehydration can sometimes affect blood pressure regulation as well.
Exercise: Move More for a Healthier Heart
Physical activity is another cornerstone of controlling hypertension. Your heart is a muscle, and exercise helps make it stronger and more efficient at pumping, which lowers the pressure on your arteries. Regular exercise also improves circulation, helps with weight control, and reduces stress hormones – all positive for blood pressure. You don’t have to become a marathon runner; even moderate activities produce benefits. Studies show that getting about 150 minutes of moderate-intensity aerobic exercise per week (for example, 30 minutes a day, 5 days a week of brisk walking, cycling, swimming, or similar activities) can lower systolic blood pressure by 5–8 mmHg on average. That’s as much as some medications, just from moving your body!
Aim to include a mix of aerobic exercise (cardio that raises your heart rate) and some strength training. Aerobic exercise has the most direct impact on lowering BP but adding 1–2 days a week of light weight training or resistance bands can further improve your vascular health and metabolism. If you’re not very active now, start small and build up gradually – even a 10-minute walk is a good start. Over time, try to sit less and move more throughout the day. Little changes like taking the stairs, doing active chores, or short walking breaks add up. Find activities you enjoy – dancing, gardening, biking, anything to get blood flowing. Consistency is key.
Always check with your doctor before starting a new exercise program, especially if your blood pressure is very high, but in general moving more is one of the safest, best things you can do for your heart.
Stress Reduction: Calming the “Fight or Flight” Response
Managing stress is a vital yet sometimes overlooked lifestyle factor in blood pressure control. When you experience stress – whether from work, personal life, or even internal physiological stress – your body responds with a surge of hormones like adrenaline and cortisol. These hormones make your heartbeat faster and constrict your blood vessels (the classic “fight or flight” response), which raises blood pressure. If you’re under chronic stress, your body may stay in a semi-stressed state all the time, keeping your blood pressure elevated continuously. This chronic activation of the stress response is harmful to your cardiovascular system over the long run.
The good news is that learning to manage stress can truly help lower your blood pressure and improve your well-being. Functional medicine often incorporates mind-body techniques to encourage a state of relaxation and balance. Some effective stress-reduction strategies include:
Mindfulness Meditation; Deep Breathing Exercises; Yoga or Tai Chi; Progressive Muscle Relaxation; and Hobbies and Leisure.
Also, social support is important. Connecting with friends or family, or talking with a therapist or counselor, can help you manage life’s challenges better, so they don’t impact your health as much. By prioritizing stress management, you’re not just helping your mental health – you’re directly helping your heart and blood vessels relax. Over time, cultivating a calmer lifestyle can lead to meaningful drops in blood pressure.
Sleep: Getting Quality Rest
Sleep is when our bodies repair and reset, and it plays a bigger role in blood pressure than you might think. Poor sleep – whether not enough hours or low-quality, fragmented sleep – is linked to higher blood pressure and makes hypertension harder to control. In fact, people with chronic sleep deprivation (regularly getting less than ~7 hours) or sleep disorders like sleep apnea have a significantly greater risk of developing hypertension. During healthy sleep, your blood pressure naturally dips by about 10-20%. If you don’t get enough rest, your BP may remain elevated around the clock. Lack of sleep also increases stress hormones and hunger hormones, which can lead to weight gain and insulin resistance – again, feeding into higher blood pressure.
Thus, prioritizing good sleep is a key lifestyle target. Most adults should aim for 7 to 9 hours of sleep per night. Here are some tips for better sleep hygiene and how it relates to blood pressure: Maintain a Consistent Schedule; Create a Calming Bedtime Routine; Limit Stimulants and Alcohol in the Evening; Ensure a Good Sleep Environment; Watch for Sleep Apnea; Treatment of obstructive sleep apnea.
By getting enough restorative sleep, you give your cardiovascular system a chance to relax each night. Many people find that improving their sleep habits leads to better energy and mood and helps bring their blood pressure down.
Supplements and Natural Aids
In addition to diet and lifestyle changes, certain nutritional supplements and herbs can support healthy blood pressure. It’s important to remember that supplements are adjuncts – they work best alongside lifestyle improvements, not as a replacement. Always consult with a healthcare provider before starting any new supplement, especially if you are on blood pressure medication (to avoid interactions or excessive lowering of BP). That said, here are a few commonly used natural aids for hypertension and how they help:
- Magnesium: Magnesium is a mineral involved in muscle relaxation and blood vessel function. A significant number of people with hypertension have inadequate magnesium intake. Supplementing magnesium can help relax blood vessels and improve blood flow.
- CoQ10: Coenzyme Q10 is a powerful antioxidant and also crucial for energy production in heart muscle cells. Some studies have found that CoQ10 supplements (around 100 mg daily) can reduce blood pressure in hypertensive patientsrupahealth.com. It’s thought to improve the energy efficiency of the heart and reduce oxidative stress in blood vessels. CoQ10 is generally very safe and also supports overall heart health.
- Omega-3 Fatty Acids: Fish oil or algae-based omega-3 supplements (high in EPA and DHA) can have a modest blood pressure lowering effect, particularly in higher doses. Omega-3s help reduce inflammation and improve artery flexibility. They also benefit triglyceride levels and brain health. If you don’t consume oily fish regularly, an omega-3 supplement could be helpful.
- Potassium: While it’s best to get potassium from diet, in some cases a healthcare provider might recommend a potassium supplement to help reach the target intake (especially if you’re on a diuretic that depletes potassium). Never supplement potassium on your own without medical advice, though, because too much can be harmful. But ensuring adequate potassium intake is crucial – it’s like the counterbalance to sodium in blood pressure control.
- Herbal Remedies: Certain herbs have traditional and some scientific support for blood pressure. For example, garlic (either fresh or in capsules) can have a mild blood pressure-lowering effect and benefits cholesterol as well. Hibiscus tea is known to act like a natural ACE-inhibitor (similar to some BP medications) and has been shown in studies to reduce blood pressure a bit when consumed regularly. Other herbs like hawthorn, celery seed extract, or beetroot juice (rich in nitrates) have been used to support blood pressure as well. Always use these with guidance, especially if combining with prescriptions.
- Stress-supportive supplements: Since stress is a big component, sometimes adaptogenic herbs like ashwagandha, rhodiola, or magnesium (again) can help the body handle stress better and indirectly aid blood pressure. Even something simple like a daily B-complex vitamin or L-theanine (an amino acid from green tea) can promote relaxation without sedation.
Keep in mind, supplements are not magic pills – their effects are usually mild to moderate. But in combination with a healthy diet and lifestyle, they can provide that extra help to nudge your blood pressure into a healthier range. It’s best to work with a knowledgeable practitioner who can tailor supplement choices to your specific needs (for example, checking your blood levels of certain nutrients to see if you’re low).
Lastly, one “supplement” to mention is water – staying well-hydrated supports good circulation and kidney function. Dehydration can cause the body to conserve sodium and constrict blood vessels, so make sure you’re drinking enough fluids throughout the day.
Conclusion: An Empowering Path Forward
Hypertension may be common, but you are not powerless against it. A functional medicine approach puts you in the driver’s seat of your health by targeting the root causes of high blood pressure with personalized lifestyle changes. By improving your nutrition, staying active, managing stress, sleeping well, and supporting your body with the right nutrients, you can make a remarkable difference in your blood pressure readings and overall well-being. Many people find that these changes not only lead to better blood pressure, but also more energy, better mood, and a healthier weight – it’s a ripple effect of positive outcomes.
If you have hypertension (or are aiming to prevent it), consider working with a qualified functional medicine practitioner or integrative healthcare provider. They can help identify your unique triggers – be it inflammation, insulin resistance, stress, or others – and guide you with a tailored plan. Small steps add up: even a few changes can start moving the needle (or in this case, the blood pressure gauge) in the right direction. Don’t be discouraged by past numbers; blood pressure is very responsive to healthy habits, so improvements are always possible.
In summary, hypertension is a serious condition but one that you can influence greatly through your daily choices. It’s never too late to start taking care of your blood pressure – your heart, arteries, brain, and kidneys will thank you! By embracing a functional medicine approach, you’re not just managing a condition, you’re transforming your health from the ground up. Take that first step today, and partner with healthcare professionals who support you in addressing the root causes. With knowledge, support, and consistent effort, you can control your blood pressure instead of it controlling you. Here’s to a heart-healthy and empowered life!
Call to Action: Ready to take control of your blood pressure? Begin incorporating some of the lifestyle tips above and reach out to a healthcare provider who understands functional medicine. Together, you can create a personalized plan to conquer hypertension naturally. Remember, your health is in your hands – and every positive change makes a difference. Don’t wait for a crisis to start caring for your blood pressure. Empower yourself now with functional medicine approaches and enjoy the benefits of better health for years to come. To learn more, or for further information, contact Dr. Erica Flores at admin@restorativecardiology.com.
References:
● American Heart Association – Life’s Essential 8: Managing Blood Pressureheart.orgheart.org
● Rupa Health – A Functional Medicine Hypertension Protocolrupahealth.comrupahealth.comrupahealth.com
● Steve Grant Health – A Functional Medicine Approach to High Blood Pressurestevegranthealth.comstevegranthealth.comstevegranthealth.comstevegranthealth.com
● Kent Cardio – Tackling Hypertension with a Functional Medicine Approachkentcardio.com
● Centers for Disease Control and Prevention – Hypertension Worldwide (Infographic
Please review our business on Google Yelp Facebook
Please visit our Members’ Area to access 100s of health and fitness topics.
Did you know you can work out and exercise with a trainer at your home, office, hotel room, or anywhere in the world with online personal training?
Like us on Facebook/Connect with us on LinkedIn/Follow us on X
Make sure to forward this to friends and followers!